Like many age-related eye conditions, glaucoma is one that few patients realize they have until permanent vision loss has already occurred. Often referred to as the secret thief of sight, vision loss is irreversible with glaucoma.
Fortunately, the talented team at Dominion Eye Care can diagnose and treat glaucoma at the earliest stages to help patients manage this eye condition and preserve their remaining vision.
What is Glaucoma?
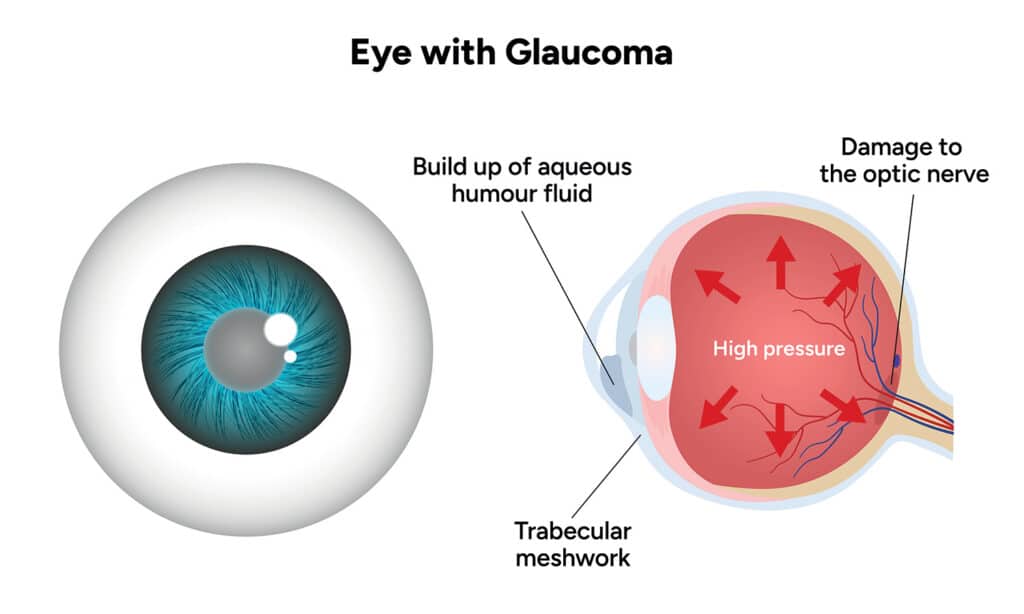
Open-Angle Glaucoma is the most common form of Glaucoma, accounting for 90% of all cases. Slow clogging of the drainage canals increases the pressure in the eye. It develops slowly and can cause irreversible damage to the optic nerve if not treated.
Open-Angle Glaucoma
Open-angle glaucoma can happen if you have a genetic trait in which the eye’s drainage openings become blocked on a microscopic level. Open-angle glaucoma is the most common form of glaucoma. Symptoms of open-angle glaucoma often take a long time to appear, meaning most patients don’t realize they have it until irreversible vision loss has already occurred.
Acute-Angle Closure Glaucoma
Acute-angle closure glaucoma is a rarer form of glaucoma caused by structural defects within the eye. Unlike open-angle glaucoma, this form of the eye condition may result in a more rapid pressure increase that can cause severe pain and other symptoms early on.
Regardless of what kind of glaucoma, the optic nerve can suffer permanent damage if the high fluid pressure isn’t lowered. The result is irreversible vision loss or even blindness.
Does Glaucoma Have Any Symptoms?
Glaucoma is often referred to as “the silent thief of sight.” This is because patients are frequently unaware they have the condition, as in its early stages, there are few noticeable symptoms that affect vision. Eventually, symptoms will arise. Those with acute angle-closure glaucoma may notice them sooner and more severely, including headache, eye pain, blurring, redness, and halos or rings around bright lights. For those with open-angle glaucoma, symptoms may appear later in the advanced stages. These include blind spots in their side vision and an increasing inability to see clearly in the center of their vision.
Typically, if a person begins to notice these symptoms, optic nerve damage may have already occurred. Your ophthalmologist can detect higher-than-usual eye pressure during an eye exam, even if you haven’t experienced any symptoms. Some patients also develop glaucoma even with pressures that are considered in a “normal” range and still require further eye pressure lowering to keep the optic nerve from deteriorating. If found early enough, regulating fluid pressure and avoiding or reducing future damage may be possible. That’s why it’s crucial to have an annual eye exam beginning by age 40 or earlier if you have a family history of glaucoma.
Treating Glaucoma
In the early stages of glaucoma, the primary treatment approach is to regulate fluid pressure through medication. The most common method for doing this is with medicated eyedrops. Prescription eyedrops help keep fluid pressure within normal ranges. However, they must be used daily to stay effective, which many patients may find burdensome. Alternatively, there are other ways to manage fluid pressure besides eyedrops, some of which involve laser or surgical procedures.
Using MIGS to Treat Glaucoma
Surgical procedures for glaucoma have been around for some time and have proven effective. They can, however, lead to a number of potential complications. Microinvasive glaucoma surgeries (MIGS) utilize equipment and techniques that operate on the microscopic level. Because they create tinier incisions than conventional surgery, they can lower the chances of complications afterward. Dominion Eye Care is one of the leading providers in the Northern Virginia region for treating glaucoma with MIGS and other procedures. We offer patients many MIGS options, including:
Treating glaucoma with one of these procedures allows patients to preserve their remaining vision and continue seeing the world.
Do you need glaucoma treatment? Learn more by requesting an appointment at Dominion Eye Care in Manassas and Warrenton, VA, today!