Diabetic Retinopathy
Around one out of ten Americans have diabetes, a health condition that prevents the body from properly regulating sugar levels in the bloodstream. This serious condition can cause problems in various parts of the body, including the eyes.
A common eye condition related to diabetes is diabetic retinopathy, which impacts more than three-quarters of diabetics. Without treatment and intervention, diabetic retinopathy can cause severe vision loss.
What is Diabetic Retinopathy?
 Diabetic retinopathy occurs when high blood sugar levels related to diabetes damage the blood vessels in the retina. The affected blood vessels can weaken, swell, leak, or even close off, depriving the retina of adequate blood flow.
Diabetic retinopathy occurs when high blood sugar levels related to diabetes damage the blood vessels in the retina. The affected blood vessels can weaken, swell, leak, or even close off, depriving the retina of adequate blood flow.
To compensate, new blood vessels may also begin to grow. Although this sounds like it could be helpful, these new vessels are weakly formed and fragile, making them a source of many issues.
They can also grow onto the retina and block its ability to receive and process light. Over time, this damage to the retina can lead to vision loss or even blindness if left untreated.
Regular eye exams are crucial for individuals with diabetes to detect and manage diabetic retinopathy in its early stages.
Does Diabetic Retinopathy Have any Warning Signs or Symptoms?
Like many other eye conditions, the effects of diabetic retinopathy tend to worsen over time. In the early stages, you may not notice huge changes in your vision.
Even so, the condition is present and must be closely monitored. As it progresses, diabetic retinopathy may begin to cause an increase in floaters, which are spots or squiggly strings that pass along their field of vision.
It may also cause blurred vision that comes and goes. Later, you may notice dark or empty spots in your vision and, eventually, a noticeable decrease in your eyesight.
Because of its progressive nature, the best outcomes for preserving sight occur when diabetic retinopathy is diagnosed and then managed from its earliest stages. It’s important for people with diabetes to have annual eye exams to detect and begin treatment as early as possible.
If you are diagnosed with diabetic retinopathy, your eye doctor will develop a treatment plan and have you come in more regularly for treatment or evaluation.
Are There Different Types of Diabetic Retinopathy?
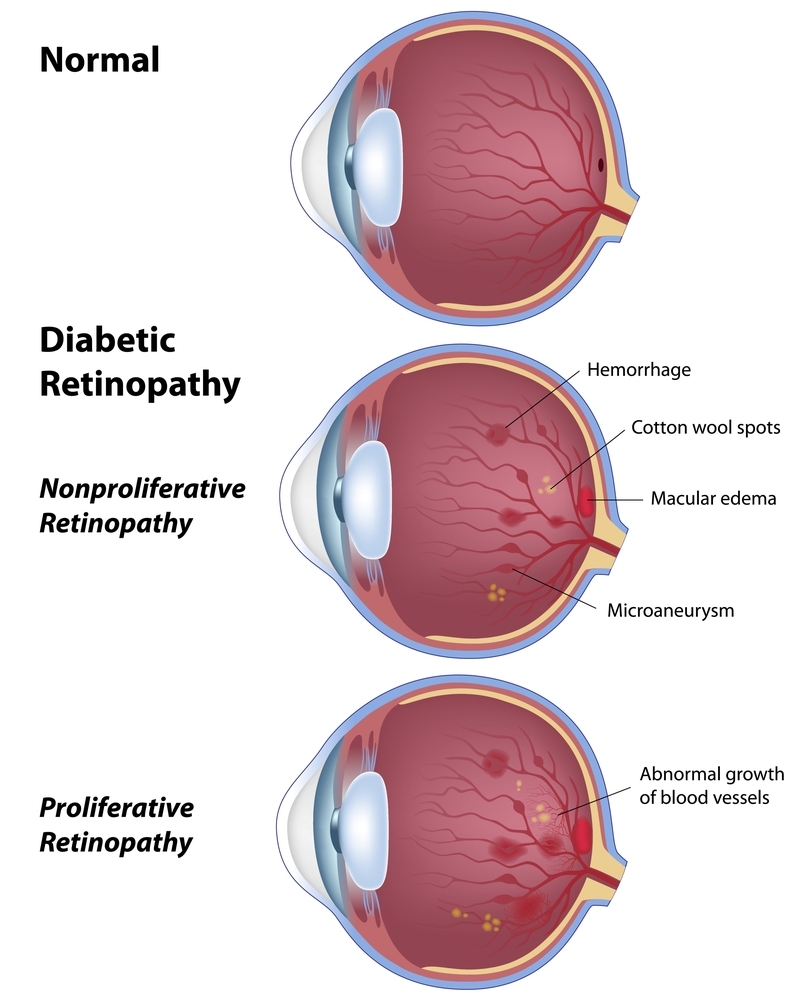
There are two main types of diabetic retinopathy, non-proliferative and proliferative. With non-proliferative diabetic retinopathy, the effects of the condition are restricted to just the area of the eye involving the retina.
If diabetic retinopathy becomes proliferative, it means the increased growth of blood vessels in the retina has moved into the vitreous, the gel-like matter that fills the inside of the eyeball. The progression of diabetic retinopathy into proliferative diabetic retinopathy can happen if blood sugar is uncontrolled. Strict blood pressure control also plays a role in limiting the development of diabetic retinopathy.
For some patients, though, their condition may remain non-proliferative, although there may still be severe consequences on the eye’s health.
Non-Proliferative Diabetic Retinopathy
It’s possible a patient with early non-proliferative diabetic retinopathy won’t notice any problems with their vision, but an eye doctor can detect the condition during an eye exam. In the milder, non-proliferative form, your eye doctor may notice tiny bulges, called microaneurysms, or some leakage in the blood vessels.
This can progress to even more microaneurysms and leakage, swelling and blockage of blood vessels, and an accumulation of fluid around the macula, a condition called diabetic macular edema. In its most severe stages, the blood vessels become blocked and decrease blood flow to the retina, to the point that new blood vessels begin to form to compensate for the decreased blood flow.
Proliferative Diabetic Retinopathy
Proliferative diabetic retinopathy is a much more advanced and severe form of the condition. In this form, aneurysms and leakage multiply, and along with it, an increase in diabetic macular edema.
As the damage worsens, one of the more severe effects of the disease may occur, which is the pulling away or detachment of the retina from its supporting tissue. Those with retinal detachment may notice light flashes, spotty vision or a noticeable loss in vision.
How is Diabetic Retinopathy Treated?
 The best treatment and management for diabetic retinopathy depends on the type, whether proliferative or non-proliferative, and its stage of progression. With early non-proliferative diabetic retinopathy, your eye doctor may determine that the condition requires regular eye exams so they can monitor any changes in your eyes or symptoms.
The best treatment and management for diabetic retinopathy depends on the type, whether proliferative or non-proliferative, and its stage of progression. With early non-proliferative diabetic retinopathy, your eye doctor may determine that the condition requires regular eye exams so they can monitor any changes in your eyes or symptoms.
Patients may also be able to slow or stop the progression of diabetic retinopathy by controlling their blood sugar levels and blood pressure through medication, proper diet, and exercise. In more advanced stages, there are procedures to minimize the effects of diabetic retinopathy.
Procedures
Some patients may be candidates for laser surgery to seal off leaking blood vessels or shrink them to prevent re-growth. Lasers can also relieve the fluid buildup associated with macular edema.
In some cases, eye doctors may recommend a surgical procedure called a vitrectomy. During this procedure, an eye surgeon removes the gel inside the eye, which is called vitreous.
These surgical treatments require highly specialized care. For that reason, Dominion Eye Care refers patients in need of laser or retinalsurgery to a retinal specialist.
Anti-VEGF Injections
New blood vessel growth that could eventually interfere with vision may happen when the retina doesn’t receive adequate blood flow due to leaking or blocked blood vessels. This growth is triggered by a signal transmitted by a protein called vascular endothelial growth factor (VEGF).
A retinal specialist can inhibit new blood vessel growth by stopping the formation of VEGF with an injection in the eye of anti-VEGF medication. Anti-VEGF medication may also aid in reducing macular swelling.
As with retinal surgery, Dominion Eye Care refers patients to a retinal specialist for anti-VEGF injections.
Do you have diabetes and want to have your eyes checked? Schedule an appointment at Dominion Eye Care in Manassas, VA, today!

